During your eye exam, your optometrist tests your vision and looks at the eye’s structures for signs of eye diseases. Among the most common are diabetic retinopathy and macular degeneration. While both these conditions can affect your central vision, diabetic retinopathy and macular degeneration are 2 distinct conditions that cause different types of damage to the eye and develop for different reasons.
If you have a family history of either disease, another health condition, or risk factors, your optometrist can monitor your eyes for early signs of these common eye conditions and provide recommendations on supporting your eye health.
What Is Diabetic Retinopathy?
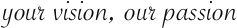
Diabetic retinopathy is a complication of diabetes that results from chronically high blood sugar levels damaging the blood vessels in the retina. The retina is the part of the eye that converts light into neural signals that the brain can interpret as vision. Diabetic retinopathy can cause blood vessels in the retina to swell or leak, leading to distorted or blurred vision.
In severe cases, it can cause the blood vessels to be damaged , resulting in the growth of new, abnormal blood vessels on the retina and bleeding, which can lead to vision loss.
Symptoms of Diabetic Retinopathy
In the early stages, diabetic retinopathy may not cause any symptoms. However, as the condition progresses, you may experience:
- Blurred or distorted vision
- Floaters—spots in your field of vision that look like little specks or strings
- Dark or empty spots in your vision
- Difficulty seeing at night
- Colour vision problems
Those with type 1, type 2, or gestational diabetes, which develops during pregnancy, should have frequent eye exams to assess the retina and other ocular structures.
The longer you have diabetes, the greater your risk of developing diabetic retinopathy, but controlling blood sugar levels can help lower your risk of the condition.

What Is Macular Degeneration?
Age-related macular degeneration (AMD) is a condition that results in the deterioration of the macula, which is the central portion of the retina responsible for sharp, central vision. It’s a leading cause of vision loss in adults and is associated with those age 50 and older.
The condition can be either dry or wet. In dry macular degeneration, tiny deposits of drusen build up in the macula, causing it to thin and break down over time. This is the most common form of AMD.
Wet macular degeneration occurs when abnormal blood vessels grow behind the retina, leaking fluid and blood and causing scarring. This can lead to distorted or blurry central vision or a blind spot in the centre of the visual field. While it’s less common, it can cause more rapid vision loss.
Symptoms of Macular Degeneration
In the early stages, macular degeneration may not cause any symptoms. However, as the condition progresses, you may experience:
- Blurred or distorted central vision
- Dark or empty spots in your vision
- Difficulty seeing fine details or reading
- Colours appearing less bright than they once did
- Vision that seems hazy or cloudy
Aging is a significant risk factor for AMD, but family history and smoking can also increase your risk. If you have risk factors, your optometrist may recommend more frequent eye exams to detect changes in your eyes before your vision is compromised.
Diabetic Retinopathy & Macular Degeneration: The Differences
Confusion surrounding diabetic retinopathy and AMD stems from questions about what part of the eye is affected by the conditions. While both occur near the retina, the location is slightly different.
Diabetic retinopathy occurs within the retina and its blood vessels, but AMD involves blood vessels or drusen that grow under the retina that don’t belong there.
Diabetic Retinopathy & Macular Degeneration: The Similarities
Treatment options for diabetic retinopathy and AMD can be similar, but there are more treatment options for diabetic retinopathy. In the early stages of AMD, your eye doctor may recommend regular checkups and monitoring of the condition.
If you have intermediate AMD, special supplements of vitamins and minerals can help slow its development to late AMD. Late dry AMD has no treatment solutions yet, however, low-vision devices can help make living with AMD easier.
Both wet AMD and diabetic retinopathy can be treated with anti-VEGF medication injections or photodynamic therapy that combines injections and laser treatment.
Corticosteroids, surgery, or other treatments can be considered for diabetic retinopathy to help manage the changes in visual acuity. Your optometrist will discuss your options with you. Preserve Your Eye Health with Regular Eye Exams
Diabetic retinopathy and macular degeneration are 2 conditions that cause eye damage and can lead to vision loss. While these are severe eye conditions, receiving an accurate diagnosis in the early stages is critical to plan the proper treatment.
Schedule an eye exam at Eye on Evanston to assess your eye structures, monitor the health of your retina, and test your visual acuity. Armed with the knowledge about your eye condition, you can secure the treatment you need to support your eye health.